Can The Endoscope Injure Sphincter ?
In rare cases, the use of an endoscope can potentially cause injury to the sphincter. However, it is important to note that endoscopic procedures are generally considered safe and complications are uncommon. The risk of sphincter injury can vary depending on the specific procedure being performed, the skill of the healthcare professional, and individual patient factors. It is always recommended to discuss any concerns or potential risks with a healthcare provider before undergoing an endoscopic procedure.
1、 Potential risks of endoscope-related sphincter injury
The use of an endoscope carries potential risks of sphincter injury, although such occurrences are relatively rare. The sphincter refers to a circular muscle that acts as a valve, controlling the opening and closing of various body passages. In the context of endoscopy, sphincter injury typically refers to damage to the gastrointestinal sphincters, such as the lower esophageal sphincter (LES) or the anal sphincter.
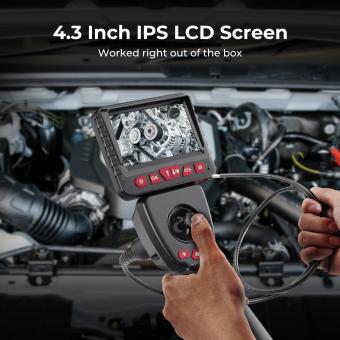
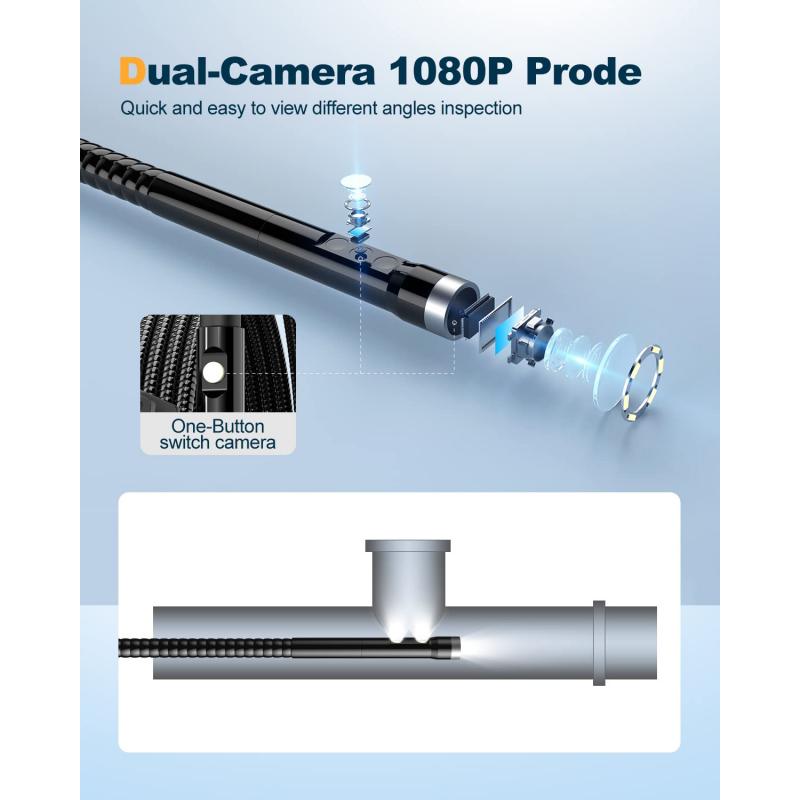
Endoscope-related sphincter injuries can occur due to various factors. One potential risk is the insertion or manipulation of the endoscope itself. The endoscope is a long, flexible tube that is inserted into the body through natural openings or small incisions. If not carefully maneuvered, it can potentially cause trauma to the sphincter muscles.
Another risk factor is the use of certain endoscopic procedures that involve the dilation or stretching of the sphincter. These procedures, such as sphincterotomy or balloon dilation, are performed to treat conditions like strictures or blockages. While they are generally safe, there is a small risk of sphincter injury during the process.
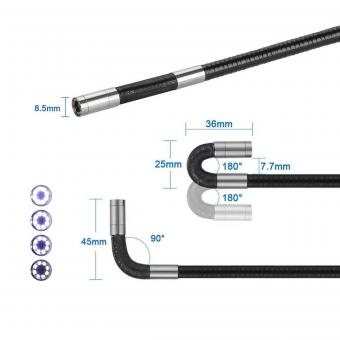
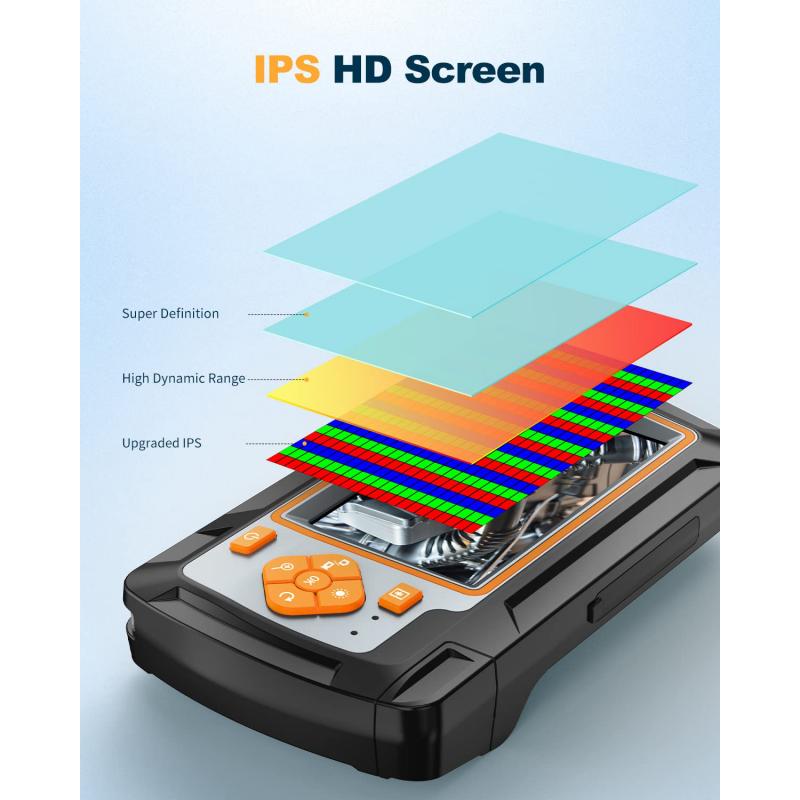
It is important to note that advancements in endoscopic technology and techniques have significantly reduced the risk of sphincter injury. The development of more flexible and smaller endoscopes allows for better maneuverability and reduces the chances of trauma to the sphincter muscles. Additionally, the use of imaging technologies, such as ultrasound or fluoroscopy, during endoscopic procedures provides real-time visualization, aiding in the safe navigation of the endoscope.
In conclusion, while there is a potential risk of sphincter injury associated with endoscopy, it is relatively rare. The advancements in endoscopic technology and techniques have greatly minimized this risk. However, it is crucial for healthcare professionals to exercise caution and expertise during endoscopic procedures to ensure the safety of patients and minimize the chances of sphincter injury.
2、 Factors contributing to sphincter injury during endoscopy
Factors contributing to sphincter injury during endoscopy can include various aspects related to the procedure itself, patient characteristics, and operator technique. While endoscopy is generally considered a safe procedure, sphincter injury can occur in certain cases.
One factor that can contribute to sphincter injury is the size and rigidity of the endoscope. Larger and stiffer endoscopes may exert more pressure on the sphincter, increasing the risk of injury. However, advancements in endoscope design have led to the development of smaller and more flexible instruments, which can help minimize the risk of sphincter injury.
Another factor is the presence of pre-existing sphincter dysfunction or pathology. Patients with conditions such as sphincter of Oddi dysfunction or previous sphincter surgery may be more susceptible to injury during endoscopy. It is important for the endoscopist to be aware of these conditions and take appropriate precautions to minimize the risk of injury.
Operator technique is also crucial in preventing sphincter injury. Proper positioning of the endoscope, gentle manipulation, and avoiding excessive force are essential to reduce the risk of injury. The use of imaging techniques, such as fluoroscopy or ultrasound, can aid in visualizing the sphincter and guiding the endoscope, further reducing the risk of injury.
Recent studies have highlighted the importance of individualized patient assessment and tailoring the endoscopic approach accordingly. Factors such as patient age, comorbidities, and anatomical variations should be taken into consideration to minimize the risk of sphincter injury. Additionally, the use of advanced endoscopic techniques, such as endoscopic retrograde cholangiopancreatography (ERCP), should be performed by experienced operators to ensure optimal outcomes and minimize the risk of complications.
In conclusion, while sphincter injury during endoscopy is a potential complication, it can be minimized by considering factors such as endoscope design, patient characteristics, and operator technique. Continued advancements in endoscopic technology and operator training are essential in further reducing the risk of sphincter injury and improving patient safety.
3、 Techniques to minimize sphincter injury during endoscopy
The use of an endoscope during medical procedures carries a potential risk of injury to the sphincter. However, there are several techniques that can be employed to minimize the risk of sphincter injury during endoscopy.
Firstly, proper patient positioning is crucial. Placing the patient in a comfortable position that allows for optimal access to the area being examined can help reduce the risk of sphincter injury. Additionally, using gentle and controlled movements during the insertion and manipulation of the endoscope can minimize the chances of accidental trauma to the sphincter.
Furthermore, the use of lubricants and local anesthetics can aid in the smooth passage of the endoscope, reducing the risk of injury to the sphincter. These substances can help to relax the sphincter muscles and make the procedure more comfortable for the patient.
In recent years, technological advancements have also contributed to minimizing sphincter injury during endoscopy. The development of smaller and more flexible endoscopes has allowed for easier navigation through the gastrointestinal tract, reducing the risk of trauma to the sphincter. Additionally, the use of imaging techniques such as ultrasound and fluoroscopy can provide real-time visualization, aiding in the precise placement of the endoscope and minimizing the risk of injury.
It is important to note that while these techniques can help minimize sphincter injury, there is still a potential risk involved. Therefore, it is crucial for healthcare professionals to undergo proper training and have a thorough understanding of the anatomy and physiology of the sphincter to ensure the safest possible endoscopic procedures.
In conclusion, while the use of an endoscope carries a potential risk of sphincter injury, there are several techniques that can be employed to minimize this risk. Proper patient positioning, gentle movements, the use of lubricants and local anesthetics, and technological advancements all contribute to reducing the chances of sphincter injury during endoscopy. However, it is essential for healthcare professionals to stay updated with the latest guidelines and advancements in the field to ensure the safest and most effective endoscopic procedures.

4、 Management of sphincter injury caused by endoscope
The use of an endoscope carries a risk of injury to various structures, including the sphincter. The sphincter is a circular muscle that helps control the opening and closing of certain body passages, such as the anus or the muscles surrounding the bile ducts. While rare, sphincter injury caused by an endoscope can occur.
The risk of sphincter injury during endoscopy depends on several factors, including the skill and experience of the endoscopist, the type of procedure being performed, and the condition of the patient's sphincter muscles. In some cases, the endoscope itself may cause direct trauma to the sphincter, leading to injury. Additionally, the insertion or manipulation of instruments through the endoscope can also potentially cause damage to the sphincter.
Management of sphincter injury caused by an endoscope typically involves a multidisciplinary approach. The initial step is to assess the extent and severity of the injury. This may involve imaging studies, such as an MRI or endoanal ultrasound, to evaluate the damage. Conservative management options, such as pain management, antibiotics, and dietary modifications, may be considered for minor injuries.
In more severe cases, surgical intervention may be necessary. Surgical repair of the sphincter injury can be performed using various techniques, including primary repair, sphincteroplasty, or sphincter reconstruction. The choice of surgical approach depends on the specific characteristics of the injury and the patient's overall condition.
It is important to note that advancements in endoscopic technology and techniques have significantly reduced the risk of sphincter injury. Endoscopists are now better equipped to visualize and navigate the anatomy, minimizing the chances of inadvertent damage. Additionally, the use of advanced imaging modalities during endoscopy, such as high-definition imaging or endoscopic ultrasound, allows for better visualization of the sphincter and surrounding structures, further reducing the risk of injury.
In conclusion, while sphincter injury caused by an endoscope is a potential risk, it is relatively rare. With proper training, experience, and advancements in endoscopic technology, the risk of such injuries can be minimized. Prompt and appropriate management, including conservative measures or surgical intervention, can help in the successful treatment of sphincter injuries caused by endoscopy.