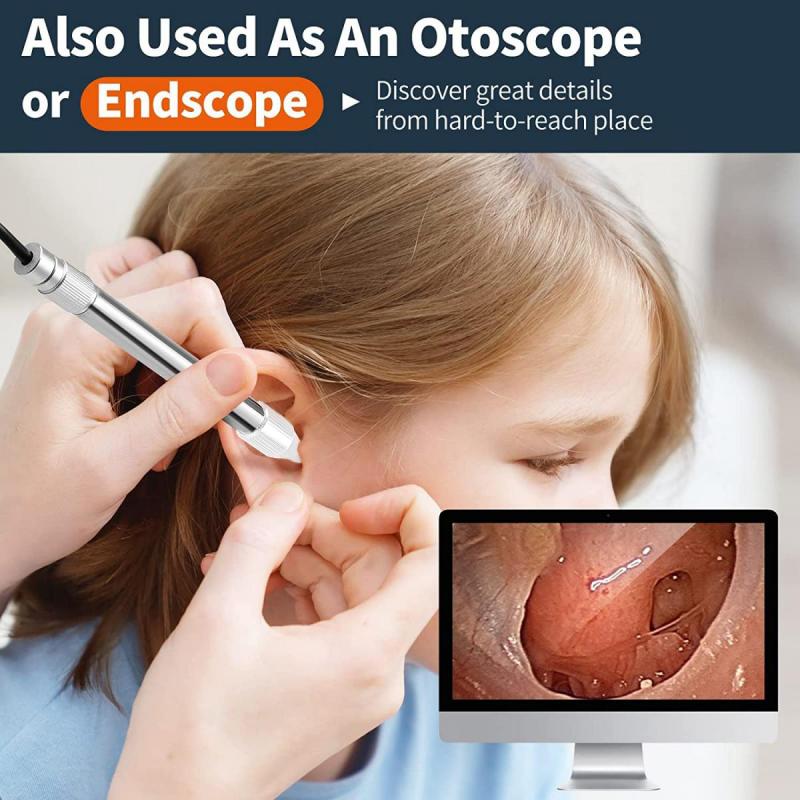
How Do They Sterilize Endoscope ?
Endoscopes are typically sterilized using a combination of high-level disinfection and sterilization techniques. The process involves several steps, including pre-cleaning, leak testing, manual cleaning, and disinfection or sterilization.
Pre-cleaning involves removing any visible debris or organic material from the endoscope. This is followed by leak testing to ensure the integrity of the endoscope's channels. Manual cleaning is then performed using enzymatic detergents and brushes to remove any remaining organic material.
After cleaning, the endoscope undergoes high-level disinfection or sterilization. High-level disinfection involves immersing the endoscope in a liquid disinfectant solution or using an automated disinfection system. Sterilization, on the other hand, involves using heat or chemical agents to eliminate all microorganisms, including bacterial spores.
The specific method used for sterilization depends on the type of endoscope and the manufacturer's instructions. Common sterilization methods include ethylene oxide gas sterilization, hydrogen peroxide gas plasma sterilization, and steam sterilization.
It is important to follow strict guidelines and protocols to ensure the effective sterilization of endoscopes and prevent the transmission of infections.
1、 Chemical disinfection methods for endoscope sterilization
Chemical disinfection methods are commonly used for endoscope sterilization. These methods involve the use of high-level disinfectants that are capable of killing a wide range of microorganisms, including bacteria, viruses, and fungi.
The process of sterilizing an endoscope typically involves several steps. First, the endoscope is thoroughly cleaned to remove any organic material, such as blood or tissue, that may be present. This is usually done by manually scrubbing the endoscope with a detergent solution and then rinsing it with water.
Once the endoscope is clean, it is immersed in a high-level disinfectant solution. The disinfectant solution is typically a chemical agent that is capable of killing microorganisms within a certain contact time. Common disinfectants used for endoscope sterilization include glutaraldehyde, peracetic acid, hydrogen peroxide, and ortho-phthalaldehyde.
The endoscope is left in the disinfectant solution for a specified period of time, usually ranging from 20 minutes to several hours, depending on the disinfectant used. After the required contact time, the endoscope is rinsed with sterile water to remove any residual disinfectant.
It is important to note that while chemical disinfection methods are effective in killing most microorganisms, they may not be sufficient to eliminate all types of pathogens, such as prions. Prions are highly resistant to chemical disinfectants and require specialized sterilization methods, such as steam sterilization or ethylene oxide gas sterilization.
In recent years, there has been a growing concern about the potential for endoscope-related infections, particularly due to the presence of biofilm. Biofilm is a slimy layer of microorganisms that can form on the surfaces of endoscopes and provide protection against disinfectants. To address this issue, new disinfection methods, such as the use of enzymatic cleaners or automated endoscope reprocessors, have been developed to improve the effectiveness of endoscope sterilization.
In conclusion, chemical disinfection methods are commonly used for endoscope sterilization. However, it is important to follow proper cleaning and disinfection protocols to ensure the effective elimination of microorganisms and reduce the risk of endoscope-related infections.

2、 High-level disinfection techniques for endoscope sterilization
High-level disinfection techniques for endoscope sterilization involve a multi-step process to ensure the elimination of microorganisms and prevent the transmission of infections. The specific steps may vary depending on the type of endoscope and the manufacturer's instructions, but generally include the following:
1. Pre-cleaning: After each use, the endoscope is thoroughly cleaned to remove any visible debris or organic material. This is typically done by flushing the channels with enzymatic detergent solutions and manually scrubbing the external surfaces.
2. Leak testing: The endoscope is then tested for leaks to ensure that it is functioning properly and there are no defects that could compromise the disinfection process.
3. High-level disinfection: The endoscope is immersed in a high-level disinfectant solution, such as glutaraldehyde or peracetic acid, for a specific period of time. This kills or inactivates a wide range of microorganisms, including bacteria, viruses, and fungi.
4. Rinse and drying: After disinfection, the endoscope is thoroughly rinsed with sterile water to remove any residual disinfectant. It is then dried using forced air or other methods to prevent the growth of bacteria.
5. Storage and transport: The sterilized endoscope is stored in a clean and dry environment to maintain its sterility until the next use. Proper handling and transport protocols are followed to prevent contamination.
It is important to note that the latest point of view in endoscope sterilization emphasizes the need for strict adherence to manufacturer's instructions and guidelines. This includes using validated disinfection solutions, following recommended exposure times, and regularly monitoring the effectiveness of the disinfection process. Additionally, there is ongoing research and development in the field of endoscope sterilization to improve techniques and reduce the risk of infections associated with endoscopic procedures.

3、 Sterilization through ethylene oxide gas for endoscopes
Sterilization of endoscopes is a critical process to ensure patient safety and prevent the transmission of infections. One commonly used method for sterilizing endoscopes is through the use of ethylene oxide (EO) gas.
Ethylene oxide gas sterilization is a low-temperature process that effectively kills microorganisms, including bacteria, viruses, and spores. The endoscope is first cleaned and rinsed to remove any organic material or debris. It is then placed in a sterilization chamber where it is exposed to EO gas. The gas penetrates the endoscope's channels and other hard-to-reach areas, ensuring thorough sterilization. The exposure time can vary depending on the specific endoscope and the manufacturer's guidelines.
After the exposure period, the EO gas is removed from the chamber, and the endoscope is aerated to remove any residual gas. This aeration process is crucial as EO gas is toxic and can be harmful if not completely removed. The endoscope is typically aerated in a well-ventilated area or a dedicated aeration cabinet to ensure the safety of healthcare workers and patients.
It is important to note that ethylene oxide gas sterilization has come under scrutiny in recent years due to its potential health and environmental risks. EO gas is a known carcinogen and can have adverse effects on human health if not handled properly. Additionally, the use of EO gas has been linked to environmental pollution and concerns about its impact on air quality.
As a result, there has been a push to explore alternative sterilization methods for endoscopes. Some of these alternatives include hydrogen peroxide gas plasma sterilization, peracetic acid sterilization, and low-temperature hydrogen peroxide sterilization. These methods offer effective sterilization while minimizing the potential risks associated with EO gas.
In conclusion, sterilization of endoscopes through ethylene oxide gas is a widely used method that effectively kills microorganisms. However, due to the potential health and environmental risks associated with EO gas, there is a growing interest in exploring alternative sterilization methods for endoscopes. Healthcare facilities should carefully consider the latest research and guidelines to ensure the safety and efficacy of their sterilization processes.
4、 Hydrogen peroxide plasma sterilization of endoscopes
Hydrogen peroxide plasma sterilization is one of the methods used to sterilize endoscopes. This process involves the use of low-temperature hydrogen peroxide gas plasma to eliminate microorganisms and ensure the endoscope is safe for reuse.
The sterilization process begins by cleaning the endoscope thoroughly to remove any visible debris or organic material. Once cleaned, the endoscope is placed in a sterilization chamber, where it is exposed to hydrogen peroxide gas plasma. The plasma is created by applying radiofrequency energy to hydrogen peroxide, which breaks it down into reactive species such as free radicals and hydrogen peroxide vapor. These reactive species then penetrate the endoscope's channels and lumens, effectively killing any microorganisms present.
The hydrogen peroxide plasma sterilization process is advantageous because it can effectively sterilize endoscopes without the use of high temperatures or toxic chemicals. It is a low-temperature process, which helps to minimize the risk of damage to delicate endoscope components. Additionally, the process is relatively quick, with a typical cycle time of around 45 minutes.
It is important to note that while hydrogen peroxide plasma sterilization is effective against a wide range of microorganisms, it may not be effective against certain types of highly resistant bacteria, such as spores. Therefore, it is crucial to follow manufacturer guidelines and recommendations for the specific endoscope being sterilized.
In recent years, there has been increased focus on the importance of proper endoscope reprocessing to prevent the transmission of infectious diseases. As a result, there have been advancements in endoscope sterilization technologies, including the use of automated systems and enhanced monitoring processes to ensure the effectiveness of sterilization. These advancements aim to improve patient safety and reduce the risk of healthcare-associated infections associated with endoscope use.